ITB pain - how does it come about?
ITB pain is pain on the outside of your knee. It's something that tends to come on gradually, generally with no clear reason - there often isn't one sudden moment where you notice it start.
It can also be quite a strong and sharp pain, which is pretty scary given you haven't done anything specific to injure it.
Some people talk about this being a friction issue, but that's not quite right. It's more an issue about compression of a small fat pad on the outside of your knee.
More than anything else, this is an issue of capacity and tolerance within your leg, leading to an irritation of this fat pad, rather than tightness or any particular damage that is occurring.
What movements aggravate it?
You'll notice it first when moving your knee from straight to bent when you're running, particularly if you're going downhill, downstairs or running with your feet in a narrow stance.
With most people, we find a change in training load tends to be what leads to this issue, especially if you're a runner.
A few key things to look out for are an increase in trail running, downhill running, or total amount of time spent training.
Technique, motor control and strength
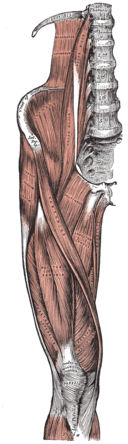
Other things we will look out for are technique issues when running - particularly how much control your hip has over your knee, alongside the strength of the key running muscles in your leg - your calf, hamstrings, quadriceps, hip flexors and glutes.
Sometimes there might be a related mobility/range of motion restriction, particularly if you lack range of motion in your ankle or hip.
Occasionally, we will see this kind of ITB pain popping up if you are having issues on the other leg, such as an old injury flaring up which might slightly change your technique.
Foam rolling won’t loosen your ITB, you don’t want it to!
A pretty common thing people try to do is to stretch or foam roll the ITB. Good luck with that!
The ITB is too strong for us to truly make any difference to it's length, plus it's designed to be tight so that it can support everything else in the leg, so we don't really want to mess with that.
Be careful foam rolling, some people find it helpful, but a lot of people find it really painful without much benefit - which makes sense if we are using the foam roller to compress the ITB, when compression of the fat pad underneath the ITB is the cause of all this pain to begin with.
You may get more benefit from using a foam roller or spikey ball around the back and side of your hip; or stretching your glutes and hip flexors, as long as getting your leg into those positions isn't painful.
Things you can do with ITB pain
As you recover from this injury, we hope to keep you moving and training as much as you can.
For runners, the best thing is to jump on the treadmill at a pretty steep incline, often this doesn't cause any issues for the knee. Otherwise there are other options for cross training like swimming, cycling, the rower or the elliptical depending on what works for you. If all else fails, a short period away from repetitive exercise will allow the tissues to settle down.
Rehab
For rehab, we divide it into two major phases.
Pain dominant phase
Here we respect the pain and inflammation around the knee and allow it space to settle, rather than pushing on with things that are making it feel worse
We will assess you, looking at strength, mobility and movement control so we know what things we need to work on to get you back to running
There will be some exercises to work on that involve your ankle, knee, hip and core all working together, but we will make sure they're happening in more comfortable positions.
Load dominant phase
This is where we begin to start loading up your hip and knee and ITB with heavier, more challenging exercises
Our goal here is to improve on what we found in our earlier assessment - likely a combination of strength, mobility and movement control
Our focus will particularly be strength, as we know that as muscles get stronger, they're able to tolerate more work, meaning running becomes a lot easier for the ITB and everything around it
What we will also do now that pain is settled is start working on a return to running program
We will play around with the distances, speeds, surfaces you are running on, plus looking at hills and stairs
It must be a gradual program that is lined up with your strengthening work, so that your knee has more capacity to handle the repetitive motion of running.
The last things we will return to in this program are downhill running and trail running as these place the most demand on the ITB
Timeline
The timeline of getting back to 100% can be quite variable. It is often dependent on how long this issue has been hanging around for, and what things we need to improve to allow the ITB to be comfortable absorbing lots of force again
Some people are back to 100% and doing everything they want after 4-6 weeks
Some people find this can hang around for a few months and that they need to be much more careful in how they progress back to what they were doing before